Due to a recent question posed in the FR and FRC Practitioner’s group, I decided instead of posting my answer to share it through our newsletter. The question had to do with the science behind performing cervical/neck CARs and how beneficial they are at increasing ROM and decreasing pain.
Having looked quickly at what some professionals say about “joint circles”, here are some “interesting quotes” to say the least…
“It is natural for your head to move in a linear fashion. Circling the head is NOT a natural movement for the neck. When you move the head in an artificial circular pattern, you override the protective mechanism that your body has in place.”
“The circling motion utilizes a combination of three different cervical ranges of motion including backwards bending of the neck, turning of the head, and side bending of the head and neck. When performed individually, these motions are harmless, as they are congruent to NORMAL cervical motion. However, danger ensues when we perform a combination of these motions simultaneously, as done when performing a neck circle.”
Yes, the quotes above are real…unfortunately….
So, joking aside, let’s get serious and set things straight as far as neck CARs. Below I have created a type of flow chart/general guidelines to follow and added recent supporting evidence:
- Take a good history (always!)
- Any recent history of dizziness, vertigo, nausea, changes in vision (diplopia), dysphagia, dysarthria, syncope
- identifying risk factors that may cause VBI such as cholesterol levels, lipids, blood sugar, blood pressure, and smoking cessation.
- questions about smoking, medications (ex. blood thinners), medical history (ex. osteoporosis, Rheumatoid Arthritis, etc)
- For the Functional Range Release practitioners
- Need to distinguish between vertigo and VBAI (needs to be done by a health-care practitioner). Vertigo by itself cannot be diagnosed as TIA or VBI. Vertigo in the presence of brainstem signs or symptoms will be diagnostic of vertebrobasilar territory TIA. Physical examination to look for brainstem signs or cranial nerve abnormalities is very important
- Assess active versus passive cervical spine ROM as per Functional Range Assessment guidelines
- Assess neck CARs
- During assessment eyes should be kept open in order to check for nystagmus
- As far as the literature when it comes to using CARs as an assessment/evaluation tool of the functional capacity of a joint refer to Summit 1 webinar
- Perform neck extension and neck rotation tests?
- “Specificity of 7 tests was sufficient, but sensitivity varied. The membranes tests had the best diagnostic accuracy, but their applicability as a test for diagnosing upper cervical spine instability in primary care has yet to be confirmed”. (Hutting et al, Phys Ther. 2013 Dec;93(12):1686-95.)
- Thus, performing these tests prior to CARs, or pre-manipulation (for those who practice chiropractic, osteopathy, or PTs that do manipulate) does not necessarily provide a clear indication. Usually done more for litigation purposes.
- Now, what else does the research show with respect to the ortho tests, end range position, and influence of position on hemodynamics of vertebral artery?
- Kranenburg R, Tyer R, Schmitt M, Luijckx GJ, van der Schans C, Hutting N, Kerry R. Effects of Head and Neck Positions on Blood Flow in the Vertebral, Internal Carotid, and Intracranial Arteries: A Systematic Review. J Orthop Sports Phys Ther. 2019 Jul 5:1-59.
- “Of the 1453 identified studies 31 studies were included and comprised data on 2254 participants. Most studies mentioned no significant hemodynamic changes during maximal rotation (n=16). A significant decrease in hemodynamics was identified for the vertebral artery with a hemodynamic decrease in the position of maximum rotation (n=8) and combined movement of maximum extension and maximum rotation (n=4). A similar pattern of decreased hemodynamics was also identified for the internal carotid and intracranial arteries. Three studies focused on high velocity thrust positioning and movement, all reported no hemodynamic changes. The synthesized data suggest that in the majority of people most positions and movements of the cranio-cervical region do not have an effect on blood flow.”
“The findings of this systematic review suggest that cranio-cervical positioning may not alter blood flow as much as previously expected.
- That is not to say that there haven’t been studies in the past indicationg a decrease in blood flow with rotation (Arnold et al, 2004; Zaina et al., 2003)
- Therefore, if maximal extension and rotation do not necessarily cause hemodynamic changes (remember this doesn’t mean we don’t assess for possible signs or symptoms), by avoiding extension, there is the potential that this can result in weakness of the neck extensors, a resultant imbalance in strength between deep neck flexors and deep neck extensors, which can potentially lead to the development of forward head carriage type position/loss of cervical lordosis due to increased activity of the neck flexors.
- Alpayci M et al. Decreased neck muscle strength in patients with the loss of cervical lordosis. Clin Biomech (Bristol, Avon). 2016 Mar;33: 98-102.
“Maximal isometric neck extension and flexion strength values were significantly lower in the patients versus healthy controls (P<0.001 and P=0.040, respectively). The mean (SD) values of the extension/flexion ratio were 1.21 (0.34) in the patients and 1.46 ± 0.33 in the controls (P=0.004). According to our results, patients with the loss of cervical lordosis have reduced neck muscle strength, especially in the extensors. These findings may be beneficial for optimizing cervical exercise prescriptions”
- Improving cervical lordosis influences cervical spine kinematics. In order to improve a loss in cervical spine lordosis, extension type exercises need to be performed.
- Moustafa IM et al. Does rehabilitation of cervical lordosis influence sagittal cervical spine flexion extension kinematics in cervical spondylotic radiculopathy subjects? J Back Musculoskelet Rehabil. 2017;30(4):937-941.
“Thirty chronic lower CSR patients with cervical lordosis < 25° were included. IRB approval and informed consent were obtained. Patients were assigned randomly into two equal groups, study (SG) and control (CG). Both groups received stretching exercises and infrared; the SG received 3-point bending cervical extension traction. Treatments were applied 3 × per week for 10 weeks, care was terminated, and subjects were evaluated at 3 intervals: baseline, 30 visits, and 3-month follow-up. Only the SG group showed a statistically significant increase in cervical lordosis (p < 0.0001). At 3-month follow up, only the SG improvements in segmental rotation and translation were maintained. Improved lordosis in the study group was associated with significant improvement in the translational and rotational motions of the lower cervical spine. This finding provides objective evidence that cervical flexion/extension is partially dependent on the posture and sagittal curve orientation.”
- Not only do extension-type exercises improve cervical spine lordosis, but they also affect vertebral artery hemodynamics in a positive manner. Therefore, training extension, whether it’s with PAILs/RAILs or CARs is very important.
- Al-Obaidi SM, Asbeutah AM, Alsiri NF. Changes in Vertebral Artery Hemodynamics Associated With McKenzie Therapeutic Cervical Movements: An Exploration Using Duplex Ultrasound Imaging. J Manipulative Physiol Ther. 2019 Jan;42(1):66-74.
“Repeated retraction with extension in a sitting position and end-range retraction with extension in supine position were significantly associated with an increase in vertebral artery volume flow. For the healthy participants in this study, McKenzie cervical movements were mostly associated with an increase in vertebral artery hemodynamics”
- The cervical spine lordosis needs to be maintained, since surprisingly, a loss of cervical lordosis is linked to decreased vertebral artery hemodynamics.
- Bulut MD, Alpayci M, Şenköy E, Bora A, Yazmalar L, Yavuz A, Gülşen İ. Decreased Vertebral Artery Hemodynamics in Patients with Loss of Cervical Lordosis. Med Sci Monit. 2016 Feb 15;22: 495-500. (FREE ARTICLE)
“The present study revealed a significant association between loss of cervical lordosis and decreased vertebral artery hemodynamics, including diameter, flow volume, and peak systolic velocity.
- Therefore, there is obviously a possibility for VBAI with maximal extension and rotation, however, there shouldn’t be a problem when performing neck CARs as long as it is done under the guidance of an #FRS practitioner and following the above rules.
- And always remember if you are not sure it’s better to refer out to someone who can clarify things for you
- I will leave you with this thought: If we were to sum up all the neck CARs ever done, all these years, up until today (which probably is a fairly large number and continuously growing), by all of our qualified FRS professionals across the world, what would be the risk factor produced? Probably very, very, low.. So just continue to use the system in order to #MSWN
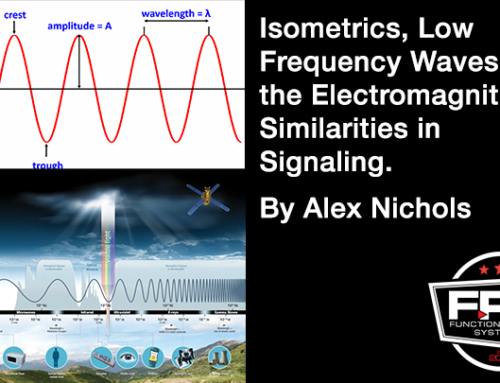
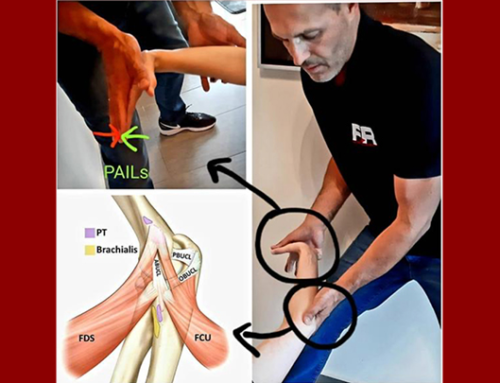
- Last but not least, there was a concern with how beneficial CARs is at increasing range of motion and decreasing pain. Remember that CARs is used in conjunction with other tools such as PAILs/RAILs to expand ROM. CARs will be critical in maintaining and expanding that range of motion (joint workspace) which will decrease pain. The study below shows how using isometric training for both cervical flexion and extension increases range of motion and consequently also decreases pain levels
Suvarnnato T, Puntumetakul R, Uthaikhup S, Boucaut R. Effect of specific deep cervical muscle exercises on functional disability, pain intensity, craniovertebral angle, and neck-muscle strength in chronic mechanical neck pain: a randomized controlled trial. J Pain Res. 2019;12:915–925. Published 2019 Mar 7.