A deeper understanding of the mechanisms behind the effects of soft tissue therapy.
By: Dr. John Saratsiotis, FRS Master Instructor
During the last few years, in the manual therapy world, we are trying to have a better and deeper understanding of the mechanisms behind the effects of soft tissue therapy. A few studies have looked at the effect of manual (soft tissue) therapy on fibrosis following either microtrauma or macrotrauma. For example, in overuse injuries research shows that the neuromyofascial system can be affected both at the acute stage (acute inflammatory cell infiltration) or the chronic stage (chronic inflammation and fibrosis).
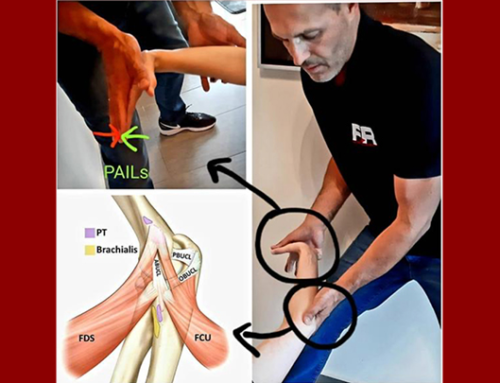
Barbe et al. investigated the effectiveness of a manual therapy (forearm skin rolling, muscle mobilization, and upper extremity traction and stretching protocols) as, what is referred to by the authors, a “preventive treatment” for rats performing an intensive lever-pulling task. Interestingly, the authors claim that they are the only laboratory performing true multimodal manual therapy on awake rats, who can provide feedback to the technician treating them.
In previous studies the authors have observed both progressively increasing sensorimotor declines and collagen production in forearm neuromuscular tissues in untreated rats performing this same arduous reaching and grasping task for 3 to 18 weeks. They have reported that a manual therapy protocol, based on a combined approach as used by many clinical manual therapists, was able to prevent these changes, when provided for 12 weeks concomitant with task performance. Specifically, they have previously reported that manual therapy of the upper extremity reduced high intensity task-induced fibrosis in extraneural, muscle, and dermal connective tissues in a long-term study, and extraneural fibrosis in a short-term study.
The results of this particular study showed that rats receiving the manual therapy showed no elevation of CD68+ or CD206+ cells (pro-inflammatory macrophages) in median nerves, flexor digitorum muscles, or flexor digitorum muscles tendons that were still involved in performing the task, and no increases in pro-inflammatory cytokines in the flexor digitorum muscles or serum.
In this current study, they observed a small but significant increase in IL-10 (a key anti-inflammatory cytokine) in TASK-Ac (task-involved lower extremities active control group) rats, compared to control rats. There was an even larger increase in muscle IL-10 in the TASK-Tx (task-involved upper extremities) rats, compared to TASK-Ac and control non-task rats. This increase in IL-10 may be inhibiting the development of tissue inflammatory responses. IL-10 also appears to have anti-nociceptive effects on muscle pain and pain due to nerve injury. Its elevation in the TASK-Tx rats may be contributing to the improved sensorimotor behavioral findings.
The authors come to the conclusion that the results provide some evidence that manual therapy, provided across several weeks during active performance of an inflammation-inducing task maintains sensorimotor function by lowering nerve, muscle, and tendon inflammation and fibrogenic processes. Research that may give us some insight as to a possible mechanism as to how manual therapy may hinder or lower fibrotic tissue production.
References
Barbe MF, Harris MY, Cruz GE, et al. Key indicators of repetitive overuse-induced neuromuscular inflammation and fibrosis are prevented by manual therapy in a rat model. BMC Musculoskelet Disord. 2021;22(1):417.
Bove GM, Delany SP, Hobson L, Cruz GE, Harris MY, Amin M, Chapelle SL, Barbe MF. Manual therapy prevents onset of nociceptor activity, sensorimotor dysfunction, and neural fibrosis induced by a volitional repetitive task. Pain. 2019 Mar;160(3):632-644.
Bove GM, Harris MY, Zhao H, Barbe MF. Manual therapy as an effective treatment for fibrosis in a rat model of upper extremity overuse injury. J Neurol Sci. 2016 Feb 15;361: 168-80.